Minutes saved mean lives saved

July 5, 1984, marked a major change in trauma care in Middle Tennessee as Vanderbilt University Medical Center launched the LifeFlight program. Before that date, people who were severely injured anywhere in the small towns, farmland and rolling hills of the region had to travel to Nashville by ground to access sophisticated, lifesaving trauma care.
At that time, there was no state-organized trauma system (that didn’t come about until 1988), so which patients were selected for transport was not uniformly defined.
Co-founded by John A. Morris Jr., MD, professor of Surgery, and the late Joseph C. Ross, MD, associate vice chancellor emeritus for Health Affairs, the LifeFlight program began as a single helicopter air ambulance service four decades ago and has grown to a comprehensive emergency medical services provider that includes critical care air and ground transport; coverage for sports and entertainment events; and emergency and dispatch communications.
Shortly after the LifeFlight program began, a paramedic in rural Clay County, Tennessee, noted that the helicopter could get a badly injured patient to Nashville in just 32 minutes, while a ground ambulance would take up to an hour and 45 minutes.
But more than that, because LifeFlight helicopters are essentially intensive care units that fly, staffed by some of the most knowledgeable trauma clinicians available, they are not just bringing the patient to the hospital, they are bringing the hospital to the patient.
Early days
Before the first flight could take off, years of dreaming and planning had to happen. The unglamorous work of obtaining permits, selecting a vendor for the aircraft, holding neighborhood meetings and securing governmental approval all had to take place.
The first helicopter — a Bell 206 LongRanger — had room for only one patient along with two flight nurses working elbow-to-elbow in the back and a pilot up front. A helicopter large enough to carry two patients at a time along with the crew — a twin-engine BK-117 — was added in 1986.

LifeFlight’s first helipad was on the south end of the Vanderbilt University Hospital Plaza, sitting approximately where the facility’s Courtyard Café is now. The Vanderbilt Clinic (TVC), where many outpatient clinics are housed on the Main Campus, hadn’t yet been built.
For a few months, as TVC construction began in 1985, flights landed at a nearby Vanderbilt University athletic field. Patients were then unloaded and transported the final few blocks by a waiting ambulance — LifeFlight’s first dedicated ground transport.
The construction of TVC brought with it the addition of a fourth-floor rooftop twin helipad, which opened for flights in late 1985. The helipad included a dedicated elevator direct to the emergency department.
In November 1991, Vanderbilt received a new BK-117 helicopter with the medical compartment’s interior custom designed by Vanderbilt flight nurses to achieve the best functionality. In April 1992, LifeFlight saw the first month of a remarkable 100 patient transports, and in the summer of 1993, the service experienced three consecutive months of more than 100 patient transports each month.
Demand leads to expansion
An ever-increasing demand for rapid transport to deliver trauma and critically ill patients to the Medical Center meant more aircraft were needed. In 1997, LifeFlight expanded operations by adding a second helicopter, LifeFlight 2, along with additional staff, including six flight nurses, five pilots, four flight coordinators and one mechanic.
To support the growing operation, the LifeFlight Skyport located on the roof of VUH was opened in 2000, with a helipad communications center and the program’s administrative offices. The communications center in the Skyport is staffed continually by EMTs or paramedics who expertly coordinate all patient transports.
As the number of flights grew, VUMC’s clinical programs responded by growing to meet the needs of the region’s trauma victims. This meant upgrading the emergency department, adding to the trauma service and eventually establishing the Department of Emergency Medicine in 1992. In 1998 the dedicated Trauma Intensive Care Unit was opened in VUH.
That same year a pediatric emergency department was added on the first floor of TVC, just across the ambulance driveway from the main VUMC emergency department. This meant that for the first time, sick and injured children in the region could receive emergency medical treatment in a separate, child-oriented environment.
Beginning in 2000, LifeFlight 2 was based at Bedford County General Hospital. This was the first of the program’s bases to be located away from the Main Campus in Nashville. Just two years later, a third LifeFlight helicopter was added at the then Gateway Medical Center in Clarksville, Tennessee.
In May 2003, a LifeFlight “hot line” yellow phone system was implemented to provide emergency medical services (EMS) agencies and hospitals throughout Middle Tennessee and southern Kentucky a direct connection to Flight Communications.
Another remarkable year for expansion of LifeFlight was 2004 as three new helicopters — American Eurocopter EC-145s — were added. They were based in Lebanon, Clarksville and Shelbyville. LifeFlight became the first hospital-based air ambulance program in North America to utilize the EC-145, then recognized as one of the safest, state-of-the-art helicopters on the market.
That same year, fixed wing transport was added to the LifeFlight program, with a flight crew available seven days a week to transport patients over a longer range. Today, LifeFlight’s Fixed Wing division transports neonatal, pediatric and adult patients, as well as high-risk
obstetrics, multisystem trauma and burn patients, and organ transplant recipients. The program also performs repatriation flights to transport patients back to their home to continue medical care.
The fixed wing aircraft is equipped with a multifunction ventilator, cardiac monitors, medical oxygen, compressed medical air, IV pumps and medications. The Fixed Wing division can transport patients with a ventricular assist device, with a VUMC cardiac perfusionist accompanying the flight team.
And the Growth Continues
The LifeFlight Event Medicine division was added in 2008 when VUMC became the official health care provider of the Nashville Predators hockey team. LifeFlight Event Medicine provides EMT and paramedic-level EMS for team members and spectators at all home hockey games. In addition, LifeFlight Event Medicine currently provides EMS coverage, including ambulance standby, for all Bridgestone Arena events, Vanderbilt University sports games, Nashville Sounds Baseball and special events such as area festivals.
LifeFlight staff in easily spotted Event Medicine uniforms and emergency transport vehicles at the ready to care for the injured or ill are now a common sight whenever crowds gather for fun. More than 14,000 entertainment, sporting and community events have been staffed by the Event Medicine crew, who have treated more than 600 patients on-site and completed more than 800 transports.
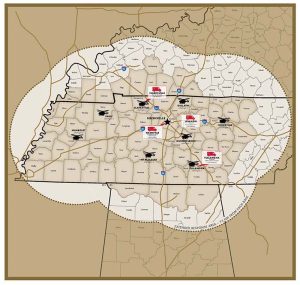
LifeFlight Ground EMS was added in 2011, and the entire fleet now includes nine helicopters, one airplane, 28 advanced life support ground ambulances and four critical care ambulances. Additional air and ground bases outside of Nashville have been established throughout LifeFlight’s coverage area in Clarksville, Cookeville, Gallatin, Humboldt, Lebanon, Mt. Pleasant, Murfreesboro, Paris and Tullahoma. The coverage area includes Middle Tennessee, parts of West and East Tennessee, southern Kentucky and northern Alabama. These air and ground bases in communities help providers reach critically injured patients even more quickly.
Today, LifeFlight operates two communications centers that are instrumental in efficiently coordinating patient care and transportation services. One center triages three helipads, provides air advisories to flight crews, and offers rapid response support to VUMC’s four Main Campus hospitals — Vanderbilt University Hospital, Monroe Carell Jr. Children’s Hospital at Vanderbilt, Vanderbilt Psychiatric Hospital and Vanderbilt Stallworth Rehabilitation Hospital.
The other communications center was established in 2018 to provide around-the-clock transportation coordination for the entire Vanderbilt Health system, including the Regional Hospitals — Vanderbilt Wilson County Hospital, Vanderbilt Bedford Hospital and Vanderbilt Tullahoma-Harton Hospital.
Vanderbilt LifeFlight’s distinctive gold, black and white transport vehicles have become a comforting presence in Tennessee. When the winged crest is spotted, the crew’s mission is clear.
And the impact of the LifeFlight program, now spanning four decades, is illustrated by a truly remarkable measure: mothers, fathers, brothers, sisters, wives, husbands, children and grandparents — alive.
Reporting by Craig Boerner, Kathy Rivers, Holly Fletcher, Erin O. Smith, Wayne Wood
