Cancer biology Ph.D. program
The Cancer Biology Graduate Program is designed to train students for a career in basic and applied cancer research, as well as in related careers associated with the application of information through biotechnology, and the dissemination of information to the next generation of scientists and to the lay public.
RESEARCH

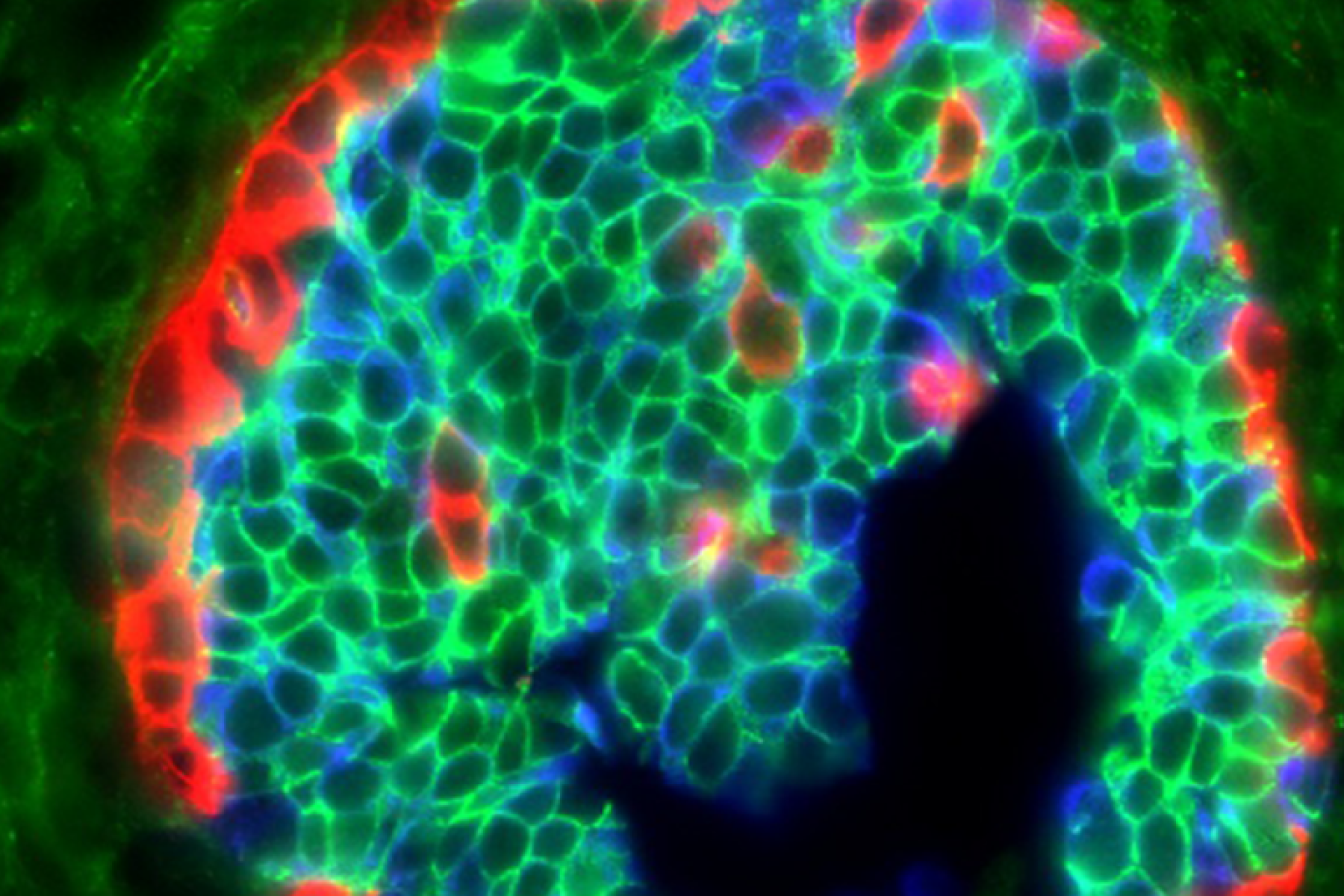
Cutting-edge research in the Program in Cancer Biology spans cancer genetics and signaling, targeted therapies and resistance pathways, precision medicine, host-tumor interactions, metastasis, exosomes and the tumor microenvironment, across multiple blood cancers and solid tumors.
program leadership

Chaired by Program Director and Director of Graduate Studies, Rachelle Johnson, the Cancer Biology Graduate Program policy is monitored and enforced by the Graduate Executive Council (GEC).
student association

The Cancer Biology Student Association (CBSA) is a student-led service organization dedicated to supporting graduate students in the Cancer Biology Program.