By Sohini Roy
Neuroblastoma, an aggressive pediatric brain cancer with a high mortality rate, boasts a unique microenvironment that puts the brakes on infiltrating immune cells and dampens their anti-tumor activities. Clinicians use a therapy called immune checkpoint blockade to activate a patient’s immune cells to recognize and attack malignant cells in many types of adult tumors. The immunosuppressive interior of neuroblastoma tumors, however, thwarts ICB.
Lihong Wang-Bishop, in the lab of John Wilson, assistant professor of chemical and biomolecular engineering, sought agents to make neuroblastoma more immunogenic or “visible” to immune cells. In a recent report in Journal for ImmunoTherapy of Cancer, Wang-Bishop and colleagues detail new insights into Stimulator of Interferon Genes, a known immune pathway for tumor detection. STING activates dendritic cells, which alert T cells to recognize and destroy cancer cells. The scientists hypothesized that STING activation could override neuroblastoma’s immune suppressive signaling, making it responsive to ICB.
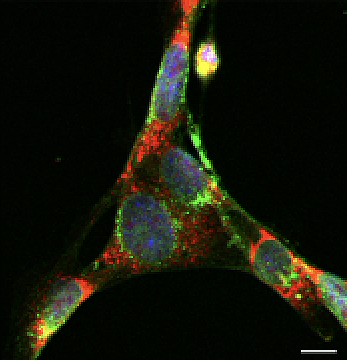
To find out, the team delivered a STING-stimulating drug encapsulated in a nanoparticle envelope that improved drug transmission across the plasma membrane to the interior of human neuroblastoma cells in cell culture. In vitro, the combination treatment activated STING, turned on inflammatory genes, and precipitated extensive cell death. The presence of STING-NP–treated tumor cells activated dendritic cells, which then efficiently engulfed the tumor cells. To validate this finding in vivo, the authors inoculated mice with tumor cells killed by in vitrotreatment with STING-NP. Next, they injected those vaccinated mice with live tumor cells. Over the span of 120 days, 50 percent of the treated mice remained tumor free; all of the non-vaccinated mice developed tumors.
In a different population of mice with neuroblastoma, intratumoral STING-NP injection activated the STING pathway and remodeled the tumor interior. STING-NP–treated tumors showed higher tumor-killing CD8+ T cells, fewer tumor-promoting regulatory T cells, and extensive immunogenic tumor cell death; the combination inhibited tumor growth and provided significant protection against recurrence. Additionally, the STING-NP–treated mice showed a heightened response to ICB therapy, increased tumor regression, prolonged survival, and a lower tumor recurrence rate. STING-NP treatment also inhibited tumor growth at sites distant from that of injection, suggesting the possibility that STING-NP treatment might reduce metastases in neuroblastoma patients.
This study shows for the first time that STING pathway activation in neuroblastoma can promote immune response. A multi-pronged approach combining a STING activator with ICB therapy has the potential to improve neuroblastoma outcomes in the clinic.
This research was supported by grants from Alex’s Lemonade Stand Foundation, the American Cancer Society, the Canadian Institutes of Health Research, Love Your Mellon, the National Institutes of Health, the National Science Foundation, the Pediatric Oncology Student Training Award, and the Stand Up To Cancer Innovative Research Grant.