Although numerous cancers are treated thanks to a vast arsenal of drugs and therapeutic strategies, the tools at our disposal sometimes fall short. In some cases, cancers develop resistance to our existing therapies, and in others, clinicians just don’t have a good way to target a particular type of malignancy. For these reasons, there is an undeniable need to increase the size and breadth of our toolset to treat cancers.

The lab of Bill Tansey, professor of cell and developmental biology and biochemistry, studies transcriptional regulation in normal and cancer cells, with a focus on the oncoprotein and transcription factor MYC. MYC controls the expression of thousands of genes linked to cell growth, proliferation, metabolism, and genome instability, and dysregulation of MYC is estimated to contribute to up to one third of all cancer deaths annually.
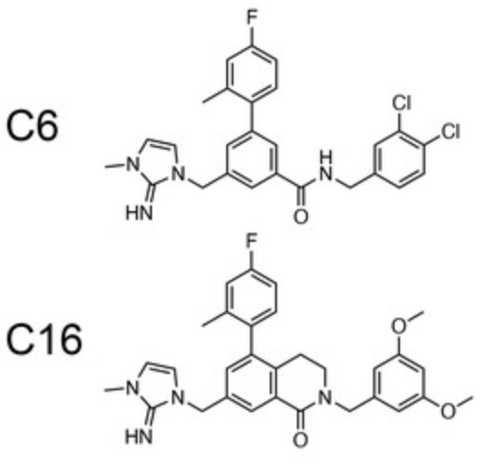
A protein called WDR5 recruits MYC to chromatin, an essential step in driving tumorigenesis. This makes WDR5 a potential target for anticancer therapies. Particularly promising is a region of the protein called the WIN site, which WDR5 uses to tether to chromatin. Inhibitors targeting the WIN site are called WINi, and they are active against multiple cancer cell lines in vitro. Although the first WINi were small, protein-like chains designed to mimic a protein ligand, the Tansey lab, in collaboration with the labs of Stephen Fesik, the Orrin H. Ingram Professor of Cancer Research and professor of biochemistry and pharmacology, and Qi Liu, professor of biostatistics, recently discovered and characterized small-molecule (drug-like) WINi.
“The mechanism of action of WINi is unclear and has been controversial,” Tansey said.
The recent paper, published in eLife and led by Research Assistant Professor of Cell and Developmental Biology Gregory “Caleb” Howard, sought to clarify the mechanism of action of the small-molecule WINi in acute myeloid leukemia cells.

“We found that WIN site inhibitors kill cancer cells by choking their ability to make ribosomes—the cellular machines that make proteins,” Tansey said. “This choke, in turn, activates a cellular response involving a protein called p53 that triggers cancer cell death.”
Cancer cells need higher levels of protein synthesis to support their accelerated growth. Some cancer therapies target this “ribosome addiction” by preventing the production of ribosomal RNA, but Tansey and colleagues are the first to describe an anticancer agent—a WINi—that blocks the production of ribosomal proteins, a new target that could be exploited to treat cancers.
“Caleb [Howard] did an amazing job spearheading this work,” Tansey said. Howard, a former graduate student in his lab, did all the “-omics” work—he profiled transcriptomes, translatomes, and proteomes of MLL-rearranged leukemias in response to the WINi. Tansey also celebrated the highly collaborative nature of the project. “The fact that we have medicinal chemists, basic scientists, and physician scientists working together, in addition to the superb shared resources we have access to at Vanderbilt, is unique,” he said.
Tansey and Fesik have been working together for a decade to target WDR5 as an anticancer strategy. Thanks to recent improvements in the inhibitors by the Fesik lab, the team has declared a clinical candidate WINi and is moving toward investigational new drug–enabling studies, an early and key part of the lab-to-bedside drug pipeline. The regulatory road that the WINi must travel before it is approved for use in the clinic is long, but the researchers hope that clarifying the mechanism of action will help accelerate its journey.
In the meantime, Tansey and colleagues are interested in determining if targeting ribosomal proteins can be used to attack other cancer types, such as colorectal cancer. “We also want to leverage our understanding of the mechanism of action to make these WINi agents more effective in the clinic, which involves selecting the patients or cancers that are the most likely to respond and figuring out what therapies WINi can be combined with to improve outcomes,” Tansey said.
Go deeper
The paper “Ribosome subunit attrition and activation of the p53–MDM4 axis dominate the response of MLL-rearranged cancer cells to WDR5 WIN site inhibition” was published in eLife on April 29, 2024.
Funding
This research was funded by the National Institutes of Health, the National Cancer Institute Experimental Therapeutics Program, the Robert J. Kleberg, Jr. and Helen C. Kleberg Foundation, the Brock Family Fellowship, and the American Society for Clinical Oncology.
Shared resources
This research made use of VANTAGE, the Digestive Disease Research Center, the Flow Cytometry Shared Resource, and the Vanderbilt Proteomics Core in the Mass Spectrometry Research Center.