Why medical students learn the Krebs cycle: A fascinating case report by alumnus Joshua Fessel, M.D., Ph.D. (’06)
by Rachel Brown (G2)
Avery-Cohen Associate College Advisor Dr. JP Arroyo and Vanderbilt MSTP alumnus Dr. Josh Fessel (’06) recently published a true case of “bench-to-bedside” in action,”Treatment of Acute Intoxication from Inhaled 1,2-Difluoroethane,” in the Annals of Internal Medicine. While I suggest reading the actual case report, not all of our subscribers may have access to the full text, so here’s a summary.
Earlier this year in the Vanderbilt emergency department, a 26-year old woman suffered acute respiratory failure following unwitnessed recreational inhaling of 1,2-difluoroethane. She had multiple cardiac arrests due to ventricular fibrillation, but ultimately an organized rhythm was achieved, and she was intubated and transferred to the Vanderbilt CVICU. There, she had an undetectable ejection fraction in the setting of biventricular standstill. The team initiated ECMO, a left-sided Impella heart pump, and continuous renal replacement therapy. However, in spite of maximal support, the patient’s heart function had still not improved at all after 36 hours.
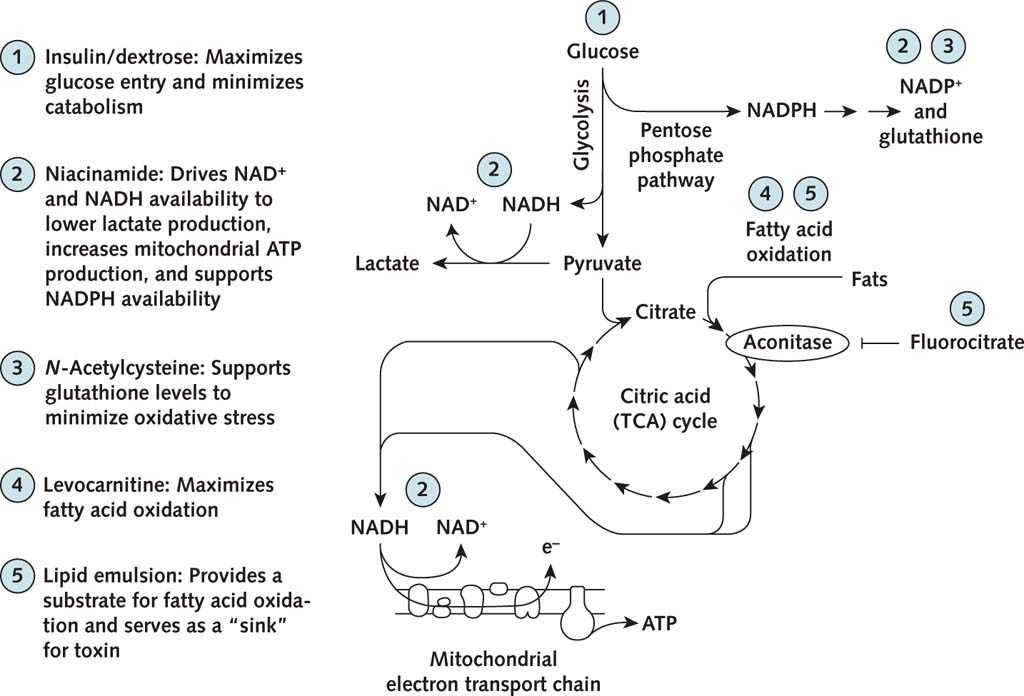
Dr. Fessel, an expert in mitochondrial and redox biology, consulted with the team. Together, they came up with a salvage therapy to attempt to restore the patient’s cardiac function based on the fact that a metabolite of 1,2-difluoroethane, fluorocitrate, blocks the citric acid cycle, halting cellular energy production. The salvage therapy consisted of: insulin and dextrose to maximize glucose entry; niacinamide to lower lactate production, increase mitochondrial ATP synthesis, and increase NADPH availability; N-Acetylcysteine to increase glutathione, an important mitigator of oxidative stress; levocarnitine to maximize fatty acid oxidation; and a lipid emulsion to provide a source of fatty acids for fuel and serve as a “sink” for the toxin. Importantly, all of these therapies were readily available in the hospital pharmacy. When asked which treatment he would prioritize, Dr. Fessel said that insulin/dextrose would be his first choice because it has been shown to improve myocardial function in other settings.
Within an hour following initiation of salvage therapy, detectable cardiac motion returned. Over the next couple of days, the patient’s ejection fraction had increased to 30% and ultimately returned to normal. However, due to multifactorial pulmonary dysfunction and severe limb ischemia secondary to venoarterial ECMO, the patient was transferred to comfort care and expired. While the salvage therapy may not have been responsible for the impressive return of cardiovascular function after complete cardiovascular collapse, there is no current antidote to 1,2-difluoroethane intoxication. Use of this therapy may be able to help other patients, particularly since the components are widely available, inexpensive, and safe to use.